Understanding Insertional Achilles Tendonitis
Do you feel a sharp pain in your Achilles tendon, making it difficult for you to carry out your daily activities? If yes, then you might be suffering from Insertional Achilles Tendonitis, a common and painful condition that can lead to long-term complications if not treated promptly.
But worry not, as this article will provide you with valuable insights and effective management techniques to help you get back on your feet. We will delve into the causes, symptoms, and various treatment options available for Insertional Achilles Tendonitis, giving you a comprehensive understanding of the condition.
Additionally, we will discuss preventive measures to help you minimize the risk of Achilles tendon injuries in the future. You will learn how to identify the warning signs of Achilles tendonitis and take preventative measures to avoid them. By following the tips and techniques outlined in this article, you can safeguard yourself against the debilitating effects of Achilles tendonitis and maintain a healthy and active lifestyle. So, let's get started and explore the nuances of Insertional Achilles Tendonitis together!
Key Takeaways
- Insertional Achilles Tendonitis is a common and painful condition that affects the Achilles tendon's lower part, making it difficult for people to carry out their daily activities.
- The condition's causes include overuse, bone spurs, poor footwear choices, foot and ankle misalignment, and participation in certain sports.
- Conservative approaches such as rest, activity modification, physical therapy, and orthotic supports are usually the first line of defense for treating Insertional Achilles Tendonitis.
The Achilles Tendon: An Overview
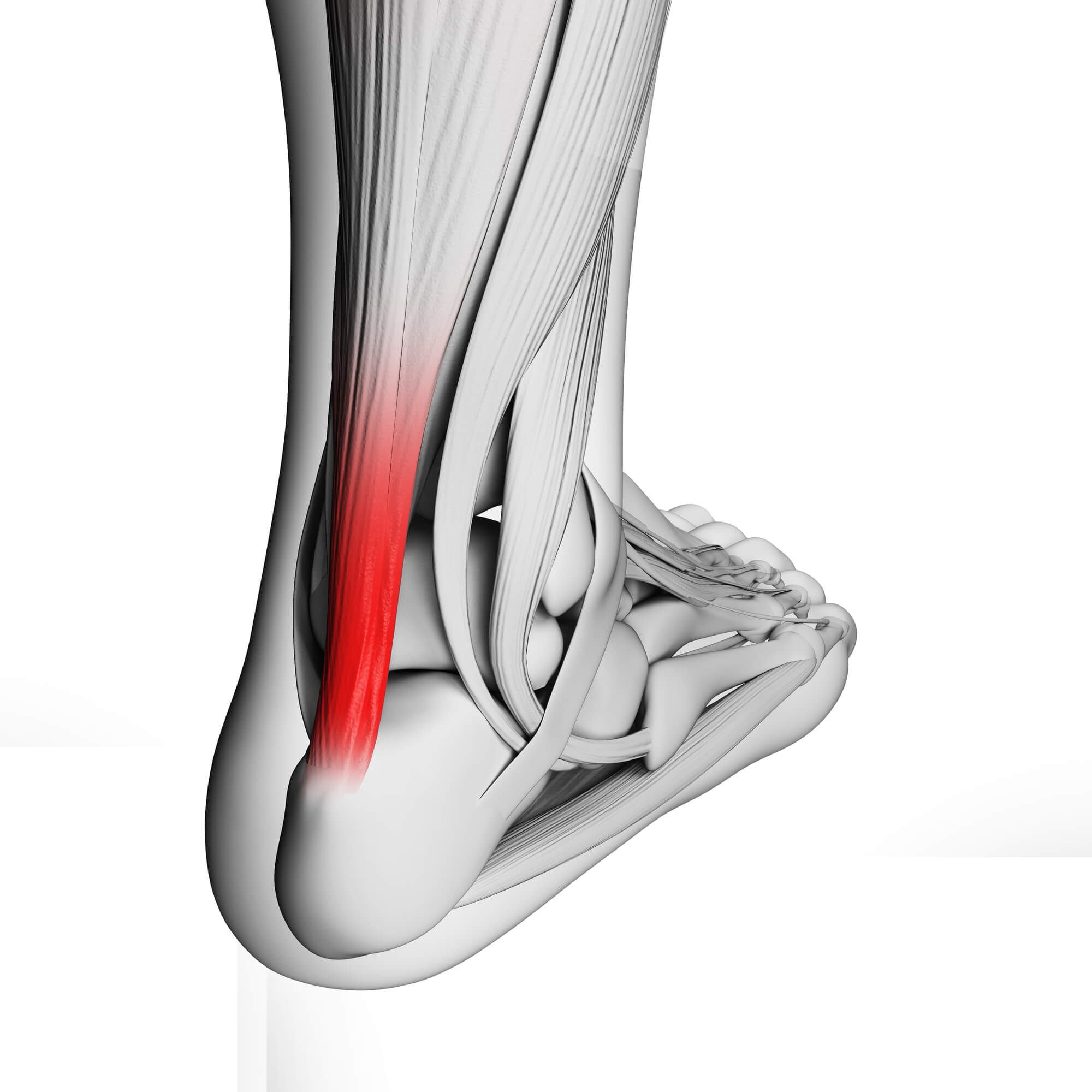
The Achilles tendon is a remarkable structure, renowned as the largest and strongest tendon in the human body. It is the essential connector between your calf muscles and the heel bone. Responsible for facilitating a wide range of movements, from walking to sports activities, the Achilles tendon is indispensable to your overall mobility.
Common Injuries to the Achilles Tendon
It is important to understand the different types of Achilles tendon injuries, such as tendinopathy, tendinosis, and tendonitis, in order to properly diagnose and treat Insertional Achilles Tendonitis.
Insertional Achilles Tendonitis Explained
Insertional Achilles Tendonitis is a condition that zeroes in on the lower part of the Achilles tendon, precisely where it inserts into the heel bone. This location is prone to inflammation and damage, often resulting from overuse or repeated stress on the tendon.
Causes and Risk Factors
Insertional Achilles Tendonitis typically takes root in scenarios involving:
- Overuse: Repetitive activities, particularly those that strain the Achilles tendon, can lead to irritation and inflammation at its insertion point.
- Bone Spurs: Bony growths, known as bone spurs, at the heel bone's insertion site can exacerbate the condition.
- Poor Footwear Choices: Ill-fitting or unsupportive shoes can contribute significantly to the development of Insertional Achilles Tendonitis.
- Foot and Ankle Misalignment: An abnormal alignment of the foot and ankle can place additional stress on the Achilles tendon.
- Participation in Certain Sports: Sports that involve frequent jumping, sudden accelerations, or abrupt changes in direction can increase the risk of developing this condition.
Signs and Symptoms
Recognizing the telltale signs and symptoms of Insertional Achilles Tendonitis is pivotal for early intervention and treatment. These symptoms may include:
- Pain and Stiffness: Persistent pain and stiffness in the back of the heel, especially notable during the morning or after periods of inactivity.
- Swelling and Inflammation: Inflammation and swelling around the area where the Achilles tendon inserts into the heel bone.
- Tenderness and Warmth: Tenderness to the touch and a sensation of warmth at the insertion site.
- Limited Range of Motion: Difficulty moving the ankle freely due to pain and stiffness.
It's important to note that distinguishing Insertional Achilles Tendonitis from other related conditions, such as bursitis or non-insertional Achilles tendonitis, requires a thorough podiatrist or healthcare professional evaluation.
Diagnosis and Evaluation
If you suspect that you may be grappling with Achilles tendon pain, seeking professional medical evaluation from a podiatrist or specialist is imperative. This evaluation typically encompasses a comprehensive physical examination, during which your healthcare provider will check for signs of tenderness and swelling and assess the range of motion of your ankle. In some cases, additional diagnostic tools such as X-rays or magnetic resonance imaging (MRI) may be recommended to gain a more detailed view of the extent of the injury.
Treatment Options
Conservative Approaches
In the initial stages of Insertional Achilles Tendonitis, conservative treatments often serve as a valuable first line of defense. These approaches aim to alleviate symptoms and promote healing without surgical intervention.
- Rest and Activity Modification: Allowing the Achilles tendon to rest and avoiding activities that exacerbate the condition is fundamental. This is often one of the first recommendations to mitigate symptoms.
- Physical Therapy: Physical therapy exercises and techniques can effectively address Insertional Achilles Tendonitis. These exercises focus on strengthening the calf muscles, improving flexibility, and reducing inflammation.
- Orthotic Support: Customized shoe inserts or orthotics can provide essential support and cushioning to alleviate pressure on the Achilles tendon.
Shockwave Therapy: A Breakthrough Treatment
Shockwave therapy represents a significant advancement in the treatment of Insertional Achilles Tendonitis. This non-invasive procedure employs high-energy sound waves to stimulate the body's natural healing response, reducing inflammation and promoting tissue repair in the Achilles tendon. It has gained recognition as an effective treatment option, particularly for cases less responsive to conservative approaches.
Medications and Injections
In certain instances, medications such as nonsteroidal anti-inflammatory drugs (NSAIDs) or corticosteroid injections may be prescribed by your healthcare provider. These medications are intended to alleviate pain and inflammation, providing relief during healing.
Surgical Intervention (if necessary)
Surgery is typically considered when conservative treatments have not yielded the desired results or in cases of severe Achilles tendon damage, including ruptures. Surgical options may involve removing bone spurs, repairing the damaged tendon, or other procedures tailored to the patient's specific needs.
Recovery and Rehabilitation
Recovery from Insertional Achilles Tendonitis varies in duration, often spanning several months. Effective rehabilitation is essential for restoring strength and function to the affected tendon.
- Timeline for Recovery: While the exact recovery timeline can differ from one individual to another, it's essential to be patient and consistent with your rehabilitation efforts.
- Physical Therapy Exercises: Physical therapy plays a pivotal role in recovery. Specific exercises, including eccentric calf strengthening exercises, are commonly prescribed. These exercises focus on rebuilding tendon strength and flexibility while minimizing re-injury risk.
- Achilles Tendinopathy Rehab: Tailored rehabilitation programs designed to address Achilles tendinopathy and its associated challenges can significantly aid recovery.

Preventing Achilles Tendon Injuries
Preventing Achilles tendon injuries and the development of Insertional Achilles Tendonitis is far preferable to dealing with the pain and inconvenience they bring. Consider the following strategies for injury prevention:
- Lifestyle Tips: Preventing overuse and allowing your Achilles tendon adequate time to recover between activities is crucial. Incorporate rest days into your routine to avoid overexertion.
- Footwear Selection: Choosing appropriate footwear is a fundamental aspect of injury prevention. Opt for shoes that provide proper arch support, cushioning, and shock absorption.
- Strengthening and Stretching: Regularly engage in exercises designed to strengthen calf muscles and improve the flexibility of the Achilles tendon.
- Professional Guidance: Athletes and individuals engaged in sports activities should consider seeking guidance from sports medicine experts. These professionals can provide valuable insights into injury prevention specific to your chosen sport or activity.
Personal Experience and Expertise
As seasoned podiatry experts, we have witnessed firsthand the challenges individuals face when dealing with Achilles tendon injuries. Our commitment to helping patients on their journey to recovery is unwavering. We understand the importance of timely intervention, personalized treatment plans, and compassionate care. If you're currently grappling with Achilles tendon pain or seeking guidance on prevention, please don't hesitate to schedule an appointment with our experienced podiatrists. We are here to provide you with the expertise and support you need to navigate your path to recovery effectively.
Conclusion
Insertional Achilles Tendonitis can be a formidable adversary, causing significant discomfort and disruption in your life. However, with the right treatment strategies and a focus on prevention, you can overcome this condition and regain mobility. Remember, early diagnosis and intervention are pivotal, so seek professional help if you suspect Achilles tendon issues. Your journey to recovery starts with the right guidance and care, and our expert podiatrists are here to guide you every step of the way. Don't let Achilles tendon pain hold you back—take proactive steps toward a pain-free and active life.
FAQ
How do you treat insertional Achilles tendonitis?
Treatment for insertional Achilles tendonitis may include conservative approaches such as rest, physical therapy, and orthotic support. In more severe cases, shockwave therapy or surgical intervention may be necessary. It's crucial to consult a podiatrist for a personalized treatment plan.
How long does insertional Achilles tendinopathy last?
The duration of insertional Achilles tendinopathy recovery varies from person to person. It often takes several months of rehabilitation and adherence to treatment recommendations. Early diagnosis and intervention can help expedite the healing process.
What exercises should you avoid with insertional Achilles tendonitis?
Exercises that put excessive strain on the Achilles tendon should be avoided. These may include high-impact activities like running or jumping. Consult with a healthcare professional or physical therapist for guidance on safe exercises during your recovery.
Is walking good for insertional Achilles tendonitis?
Walking can benefit from insertional Achilles tendonitis if done with caution and within pain tolerance. However, it's crucial to modify your walking routine, wear appropriate footwear, and follow any recommendations from your healthcare provider to avoid aggravating the condition.
Does insertional Achilles tendinopathy go away?
With appropriate treatment, including rest, physical therapy, and other interventions, insertional Achilles tendinopathy can improve significantly. In some cases, it may fully resolve; in others, it may require ongoing management. Early diagnosis and treatment offer the best chances of successful recovery.
What are the surgical options available to treat Insertional Achilles Tendonitis?
Surgical options for treating Insertional Achilles Tendonitis may include procedures such as:
- Tendon Debridement involves removing damaged or degenerated tendon tissue to promote healing.
- Bone Spur Removal: If bone spurs contribute to the condition, they may be surgically excised.
- Tendon Reattachment: In cases of severe tendon damage or rupture, surgical reattachment of the tendon to the heel bone may be necessary.
- Gastrocnemius Recession: This procedure lengthens the calf muscle to reduce tension on the Achilles tendon.
The specific surgical approach will depend on the severity of the condition and the individual patient's needs, and it should be discussed in detail with a qualified orthopedic surgeon or podiatrist.

