Managing Foot Pain in Diabetes Patients
Diabetes is a chronic disease that affects millions of people worldwide. It occurs when the body cannot properly produce or use insulin, a hormone that regulates blood sugar levels. People with diabetes are at an increased risk for various health complications, including foot problems. Diabetes can cause nerve damage, also known as diabetic neuropathy, leading to foot pain and other symptoms.
What Is Diabetes?
Diabetes is a disease in which the body cannot properly produce or use insulin, a hormone that regulates blood sugar levels. There are two main types of diabetes: type 1 and type 2. Type 1 diabetes is an autoimmune disease in which the body's immune system attacks and destroys the cells that produce insulin. Type 2 diabetes is the most common form of diabetes and occurs when the body cannot use insulin properly.

How Diabetes Affects the Feet
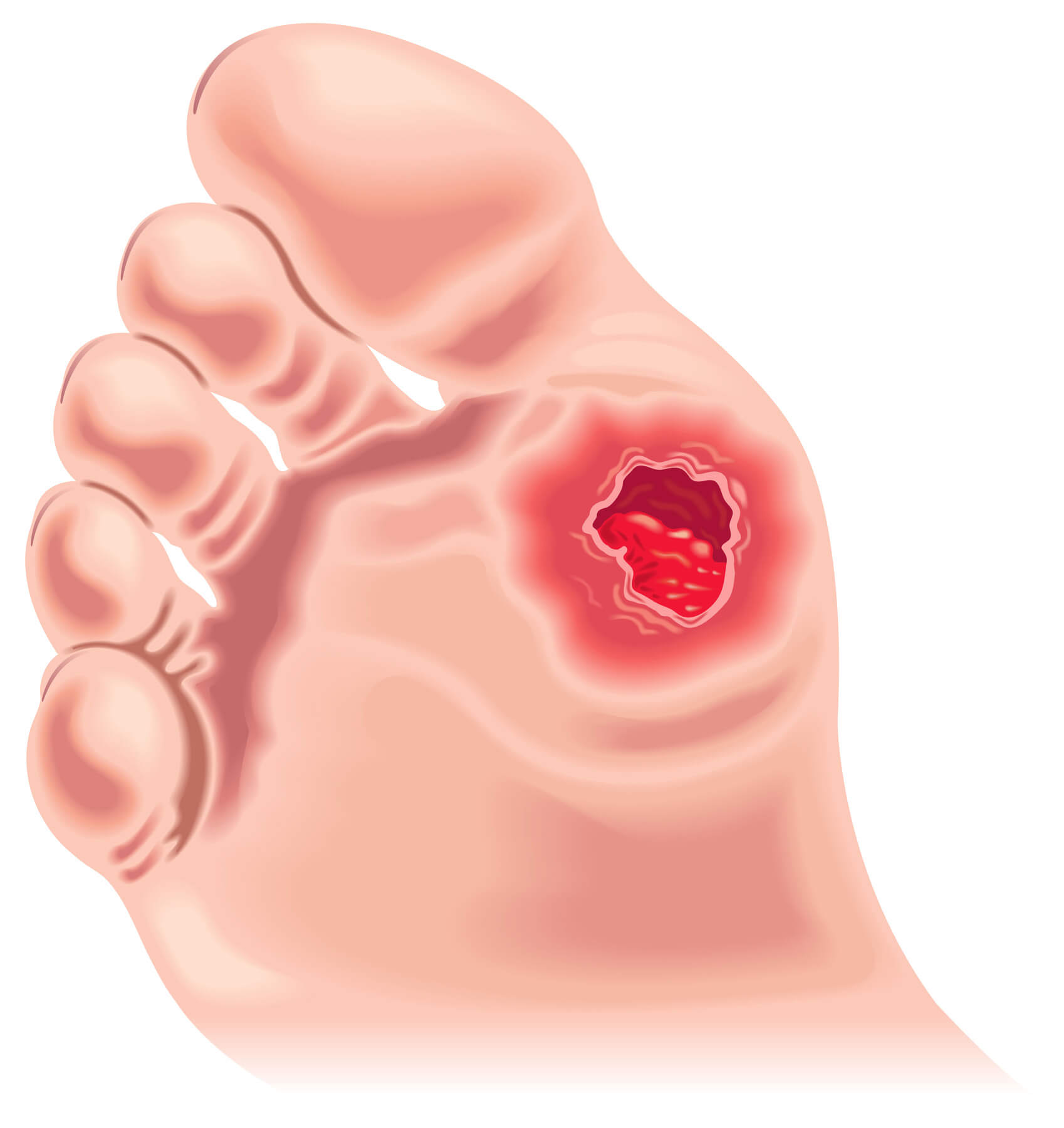
Diabetes can affect the feet in several ways. One of the most serious complications of diabetes is diabetic neuropathy, a condition that occurs as a result of nerve damage. Diabetic neuropathy can cause a loss of feeling in the feet, making it difficult for people with diabetes to feel pain, heat, or cold. This can lead to injuries, such as cuts and blisters, that go unnoticed and can become infected. Diabetic neuropathy can also cause the blood vessels in the feet to narrow, reducing blood flow and making it more difficult for injuries to heal. This can increase the risk of foot ulcers, a serious and potentially debilitating complication. Additionally, diabetes can also cause nerve pain in the feet, a condition called peripheral neuropathy, which can be debilitating.
Understanding Foot Pain in Diabetes
Common Causes of Foot Pain in Diabetes
Some common causes of foot pain in diabetes include nerve damage, poor circulation, and injuries. Diabetic neuropathy can cause a loss of feeling in the feet, making it difficult to feel pain, heat, or cold. This can lead to injuries, such as cuts and blisters, that go unnoticed and can become infected. Poor circulation can make it more difficult for injuries to heal, leading to foot pain. Injuries to the feet can also cause foot pain, especially in people with diabetes who have a loss of feeling in their feet.
Risk Factors for Foot Pain in Diabetes
Risk factors for foot pain in diabetes include poor blood sugar control, smoking, high blood pressure, and a family history of diabetes. People with poor blood sugar control are at an increased risk for diabetic neuropathy, which can cause foot pain. Smoking can reduce blood flow to the feet, making it more difficult for injuries to heal and increasing the risk of foot pain. High blood pressure can also affect blood flow to the feet and increase the risk of foot pain. A family history of diabetes can increase the risk of developing the disease, leading to foot pain.
Symptoms of Foot Pain in Diabetes
Symptoms of foot pain in diabetes include a burning or tingling sensation, numbness, sharp or shooting pain, and weakness in the feet. People with diabetic neuropathy may also experience a loss of feeling in the feet and have difficulty feeling pain, heat, or cold. These symptoms can be debilitating and make it difficult for people with diabetes to perform their daily activities.
Prevention and Treatment
Daily Foot Care Routine
One of the best ways to prevent and manage foot pain in diabetes is to establish a daily foot care routine. This should include checking your feet daily for cuts, blisters, sores, or other injuries. It is also important to wash your feet every day and dry them thoroughly, especially between the toes. This can help prevent infections and other complications. Additionally, it would be best to moisturize your feet daily to keep them soft and supple.
Wearing Proper Footwear
Proper footwear is also important for preventing and managing foot pain in diabetes. It is important to wear shoes that fit well and provide proper support for your feet. This includes shoes with a wide toe box, adequate arch support, and a low heel. Avoiding shoes with high heels, thin soles, or shoes that do not provide proper support can help prevent foot pain. You should also avoid going barefoot, as this can increase the risk of foot injuries.
Medications and Therapies
If you are experiencing foot pain due to diabetes, your doctor may recommend medications or therapies to help manage the pain. This can include over-the-counter pain relievers, ibuprofen, and prescription medications, such as tricyclic antidepressants or anticonvulsants, which can help relieve nerve pain. In some cases, physical therapy or other forms of rehabilitation can also help manage foot pain.
Surgery as A Last Resort
Surgery may sometimes be necessary to manage foot pain in diabetes. This is typically only recommended as a last resort and may include procedures such as nerve decompression surgery or amputation. Your doctor will discuss surgery's potential risks and benefits with you, to help you make an informed decision.
Conclusion
Proper foot care is essential for preventing and managing foot pain in diabetes. By establishing a daily foot care routine, wearing proper footwear, and working with your doctor to find the right medications or therapies, you can help keep your feet healthy and manage any pain resulting from your diabetes.
FAQ
How do you stop diabetic feet from hurting?
There are several ways to prevent and manage foot pain in diabetes:
- Establish a daily foot care routine that includes checking your feet every day for cuts, blisters, sores or other injuries, washing and drying them thoroughly, and moisturizing your feet daily.
- Wear footwear that fits well and provides proper support for your feet, including shoes with a wide toe box, adequate arch support, and a low heel.
- Work with your doctor to find the right medications or therapies to help manage the pain, such as over-the-counter pain relievers or prescription medications.
How do you treat diabetic foot pain naturally?
Some natural ways to treat diabetic foot pain include:
- Massaging the affected area to increase blood flow and decrease pain
- Soaking your feet in warm water with Epsom salt
- Applying heat or cold to the affected area
- Stretching and exercises to help maintain range of motion
- Acupuncture or other forms of alternative medicine.
How do I stop diabetic foot pain at night?
To stop diabetic foot pain at night:
- Establish a bedtime routine that includes a relaxing activity
- Avoid sleeping on the affected foot
- Use pillows to elevate the affected foot
- Use a heating pad or a cold pack to help reduce pain
- Consider using a supportive mattress
- Try over-the-counter pain relievers before bed
Why do diabetic's feet hurt so much?
Diabetic feet can hurt due to the complication of diabetic neuropathy, which is a condition caused by nerve damage due to diabetes. This can lead to a loss of feeling in the feet, making it difficult to feel pain, heat, or cold. This can lead to injuries, such as cuts and blisters, that go unnoticed and can become infected. Poor circulation can make it more difficult for injuries to heal, leading to foot pain. Additionally, diabetes can also cause nerve pain in the feet, which can be debilitating.
What helps severe diabetic foot pain?
Severe diabetic foot pain can be treated by:
- Medications such as over-the-counter pain relievers or prescription medications to help relieve the pain
- Physical therapy or other forms of rehabilitation
- Surgery as a last resort, in some cases, nerve decompression surgery or amputation
- Establishing a daily foot care routine
- Wearing proper footwear
- Work with your doctor or a podiatrist to find the right treatment plan.

