Blister vs. Ulcer
Blisters and ulcers are two common skin conditions that can affect the feet, causing discomfort and pain. While they may share some similarities, it's essential to understand their differences to ensure proper diagnosis and treatment. For people with diabetes, foot ulcers can be particularly concerning, as they can lead to serious complications such as nerve damage, infection, and even amputation. This article will explore the causes, symptoms, and treatment options for blisters and ulcers, focusing on diabetic foot ulcers. We'll also provide tips for preventing and managing these conditions to maintain healthy and happy feet.
Causes of Blisters
Blisters on the feet can be caused by a variety of factors, including:
- Friction and pressure on the skin: Friction and pressure can cause blisters, especially if the shoes are too tight or the feet are wet for an extended period. When the skin rubs against the shoe or another surface, it can cause a small tear in the top layer of the skin, forming a blister.
- Exposure to heat or cold: Exposure to extreme temperatures can cause blisters on the feet. For example, walking barefoot on hot pavement or wearing shoes too tight in cold weather can cause blisters.
- Chemical exposure or irritants: Chemicals, such as detergents or solvents, can cause blisters on the feet if they come into contact with the skin. Certain materials, such as latex, can also cause an allergic reaction, leading to blisters.
- Infections: Infections like athlete's foot or bacterial infections can cause foot blisters. Diabetics are at higher risk of developing infections due to nerve damage and poor circulation.
Symptoms of Blisters
The symptoms of blisters on the feet may include:
- Fluid-filled sacs on the skin
- Pain or tenderness in the affected area
- Redness or swelling around the blister
- Sensitivity to touch or pressure

Causes of Ulcers
Ulcers on the feet are usually caused by pressure or trauma to the skin, especially in people with diabetes. Other causes of foot ulcers include:
- Infections: Infections, such as foot fungus or bacterial infections, can lead to the development of ulcers on the feet. These infections can be more severe in diabetics, leading to more significant complications.
- Vascular or circulatory problems: People with diabetes are at higher risk of developing circulatory problems, which can cause foot ulcers. Poor blood flow can cause tissues to die, leading to an ulcer.
- Chronic diseases such as diabetes or rheumatoid arthritis: Diabetics are at higher risk of developing foot ulcers due to nerve damage, poor circulation, and other complications. Rheumatoid arthritis can also increase the risk of developing ulcers.
- Medications or radiation therapy: Certain medications or radiation therapy can increase the risk of developing foot ulcers, especially in diabetrics.
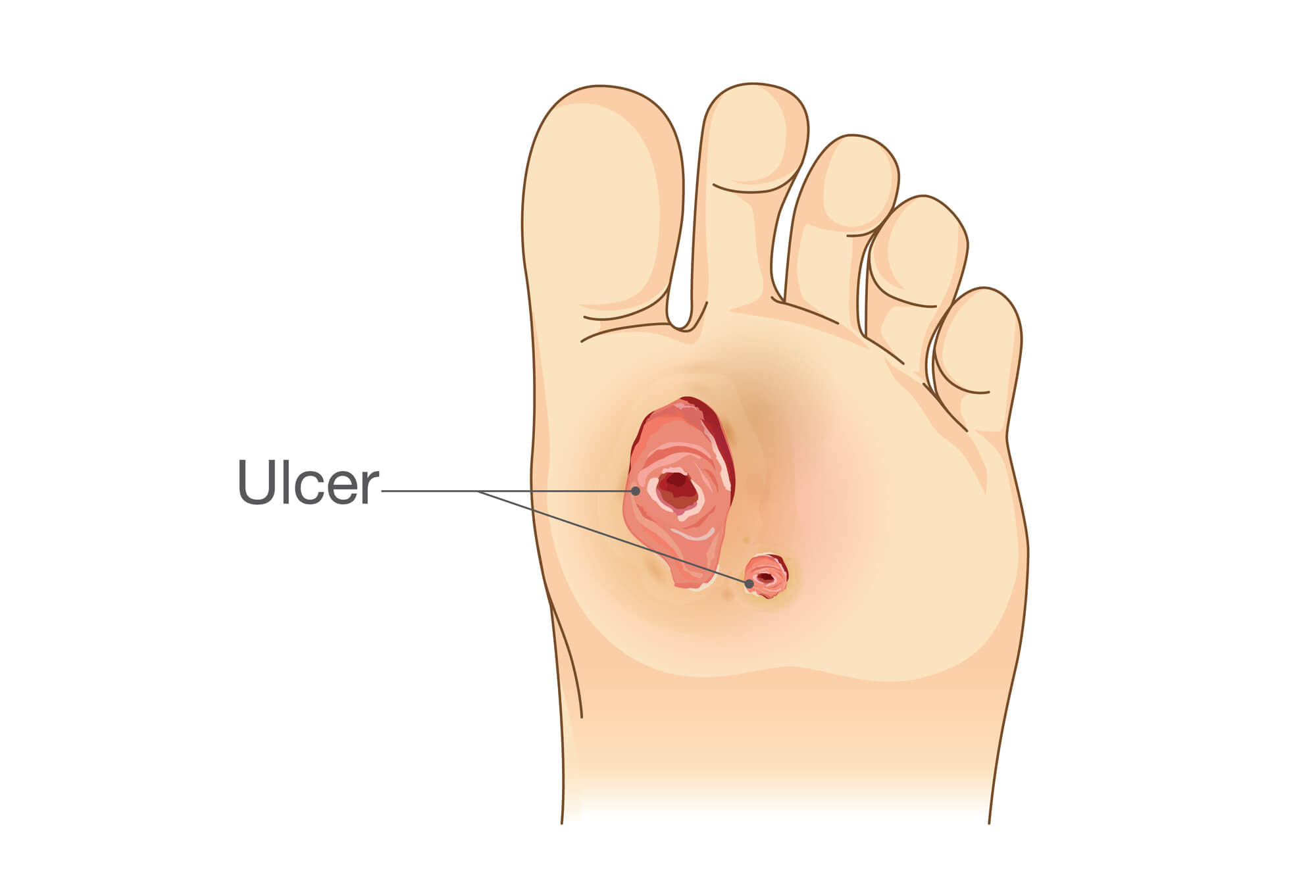
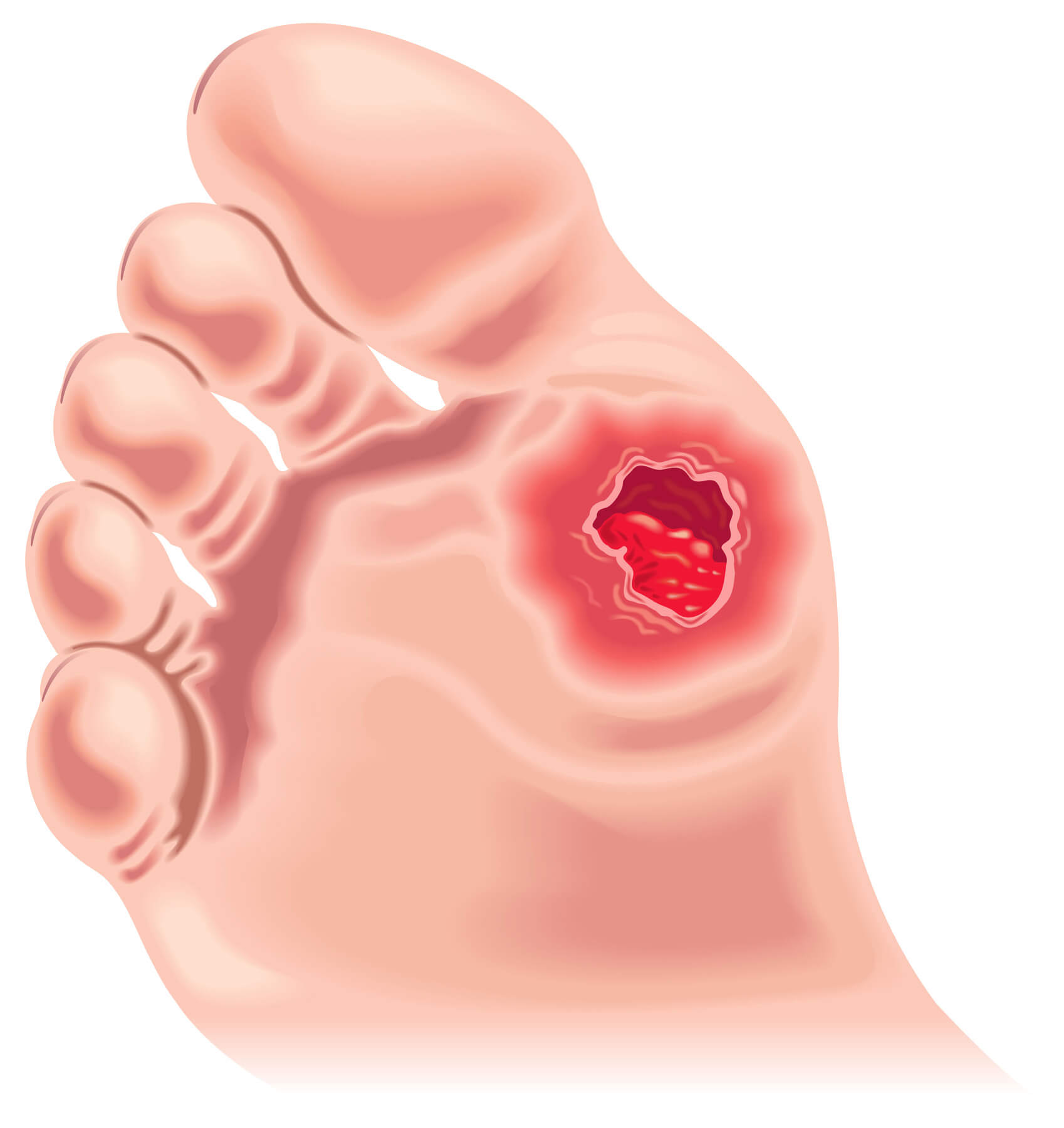
Symptoms of Ulcers
The symptoms of foot ulcers may include:
- Open sores or wounds on the skin
- Pain or tenderness in the affected area
- Drainage or pus from the ulcer
- Redness or swelling around the ulcer
- Foul odor or signs of infection
Differences Between Blisters and Ulcers
While blisters and ulcers share some similarities, the two have important differences. Blisters are usually smaller and more superficial than ulcers, typically healing within a few days. On the other hand, Ulcers can be deeper and more serious and may take weeks or even months to heal.
Another important difference is the underlying causes of blisters and ulcers. Blisters are usually caused by external factors, such as friction or pressure, while various internal and external factors, including nerve damage, poor blood flow, and infections, can cause ulcers.
Diagnosis and Treatment of Blisters
A podiatrist can diagnose and treat most blisters during a physical examination. The podiatrist will evaluate the size and location of the blister, as well as any underlying causes or risk factors. Treatment options may include draining the blister, applying topical antibiotics or other medications, and providing guidance on proper foot care to prevent future blisters.
Diagnosis and Treatment of Ulcers
Foot ulcers require more intensive diagnosis and treatment than blisters. A podiatrist will perform a thorough physical examination to determine the size and depth of the ulcer, as well as any underlying causes or risk factors. They may also perform tests to evaluate the affected area's blood flow and nerve function.
Treatment options for foot ulcers may include debridement (removal of dead tissue), dressings or wraps to protect the ulcer and promote healing, antibiotics to treat any underlying infections, and surgery to remove any dead tissue or to correct any foot deformities that may be contributing to the ulcer. It is important to seek medical attention for foot ulcers as soon as possible, as they can lead to serious complications if left untreated.
Diabetic Foot Ulcers
For people with diabetes, foot ulcers are a particularly concerning issue. Diabetes can cause nerve damage and poor blood flow to the feet, increasing the risk of developing foot ulcers. Additionally, they may have difficulty healing from foot ulcers, increasing the risk of infection and other complications.
Prevention is key when it comes to diabetic foot ulcers. Diabetics should take extra care to monitor their feet daily, looking for any signs of blisters, sores, or other issues. They should also practice good foot hygiene, keeping their feet clean and dry and wearing properly fitting shoes and socks to avoid friction and pressure. Regular check-ups with a podiatrist are also important, as they can detect any issues early on and provide guidance on proper foot care.
Conclusion
Blisters and ulcers are two common skin conditions that can affect the feet. While they share some similarities, important differences between the two can impact their diagnosis and treatment. For people with diabetes, foot ulcers can be particularly concerning, as they can lead to serious complications. People can maintain healthy and happy feet by taking steps to prevent blisters and ulcers and seeking medical attention when necessary.

