Understanding and Treating Foot Ulcers
Foot ulcers are open sores that can occur on the feet of people with diabetes or other medical conditions that affect blood flow to the lower extremities. These wounds can be difficult to heal and, if left untreated, can lead to serious complications such as amputation. It is important for people with diabetes and those at risk for foot ulcers to understand the causes and symptoms of these wounds and how to prevent and treat them effectively.
What are Foot Ulcers?
Definition and Causes
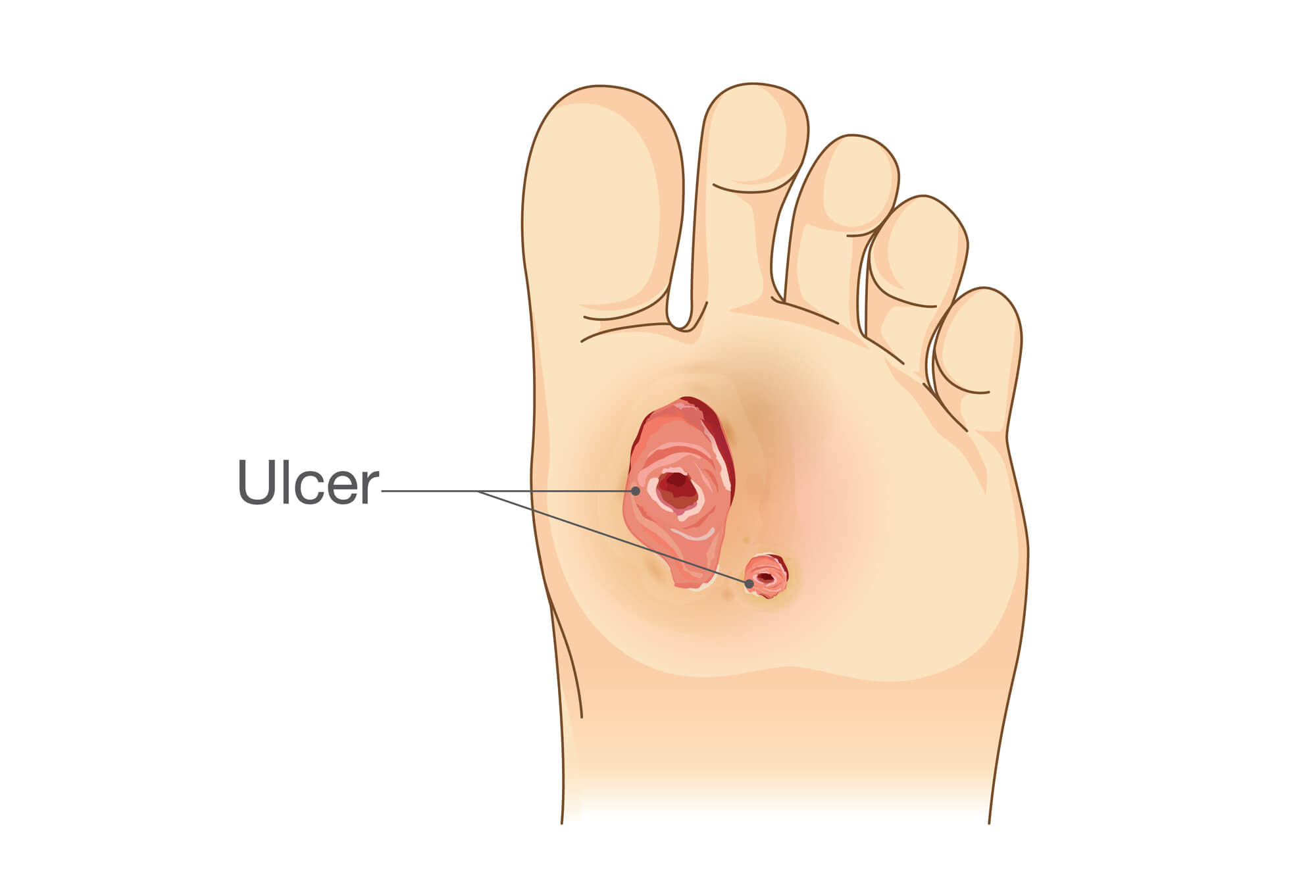
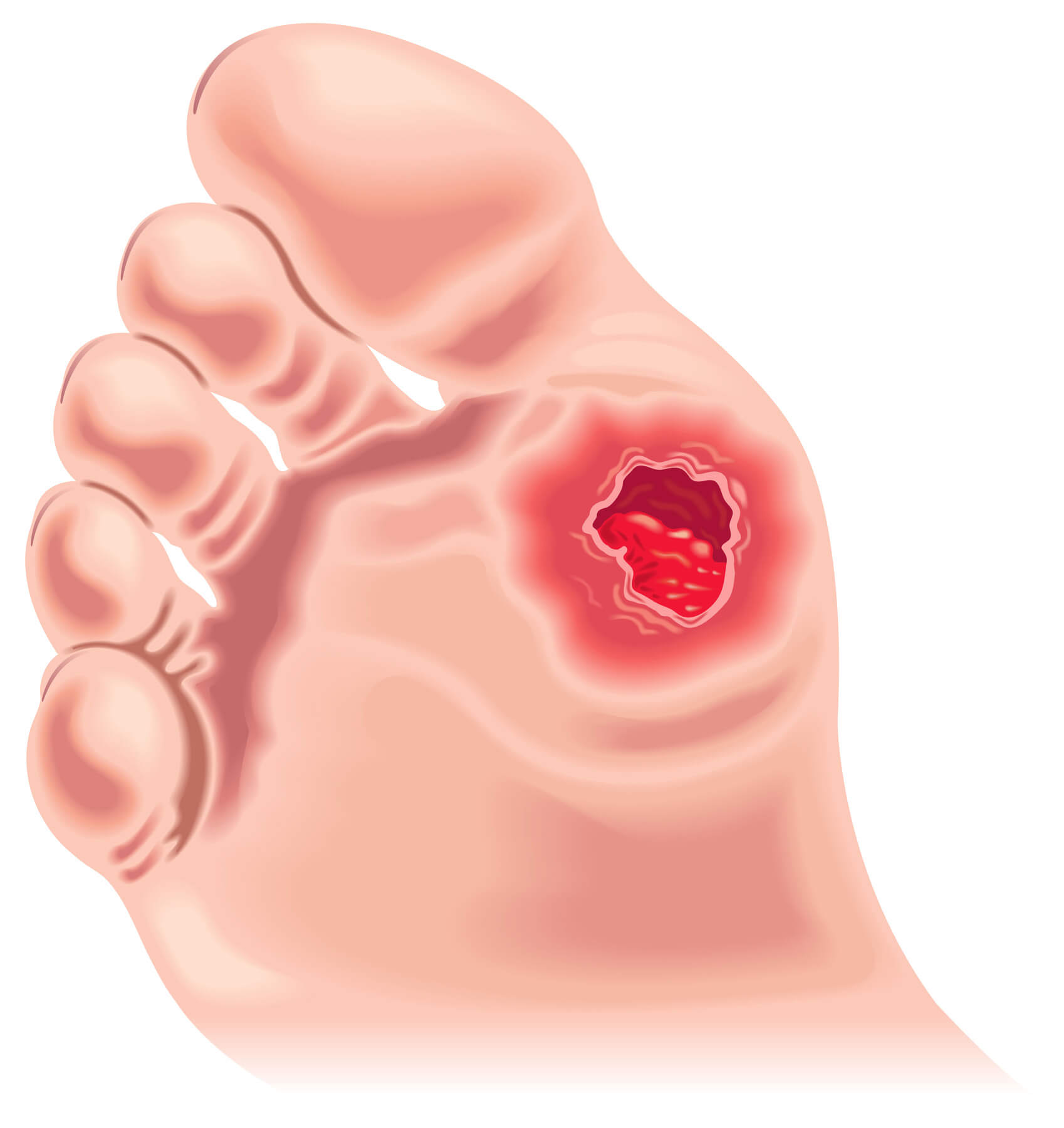
A foot ulcer is a sore or wound on the foot that does not heal within a few weeks. These wounds can range in size and depth, and they may be painful or painless, depending on the underlying cause. Foot ulcers are most commonly seen in people with diabetes, but they can also occur in individuals with poor circulation, nerve damage, or other conditions that affect the feet.
Foot ulcers are caused by a variety of factors, including:
- Trauma or injury to the foot
- Friction or pressure on the skin from poorly fitting shoes or from walking or standing for long periods
- Infection
- Poor hygiene
- Dry, cracked skin
Risk Factors
People with diabetes are at particularly high risk for developing foot ulcers because high blood sugar levels can damage the blood vessels and nerves in the feet. This can lead to poor circulation and neuropathy, making it difficult for the body to detect foot injuries or infections.
Other risk factors for foot ulcers include:
- Age: Older adults are more prone to foot ulcers due to decreased blood flow to the lower extremities.
- Obesity: Excess weight puts additional pressure on the feet, increasing the risk of developing ulcers.
- Smoking: Smoking reduces blood flow to the feet, making it more difficult for wounds to heal.
- Peripheral arterial disease (PAD): PAD is a condition in which the blood vessels in the legs become narrow or blocked, reducing blood flow to the feet.
Symptoms of Foot Ulcers
The most common symptom of a foot ulcer is an open sore or wound on the foot that does not heal within a few weeks. Other symptoms may include:
- Redness or swelling around the wound
- Pain or tenderness
- Discharge or drainage from the wound
- A change in the color or temperature of the skin around the wound
If you notice any of these symptoms, it is important to seek medical attention as soon as possible. Foot ulcers can become infected and lead to serious complications if not treated promptly.
Diagnosing Foot Ulcers
If you suspect a foot ulcer, you must see a doctor or podiatrist for a proper diagnosis. The healthcare provider will perform a physical exam of your foot and may also order one or more of the following tests:
Physical Exam
During the physical exam, the healthcare provider will carefully examine the foot for signs of infection or other complications. They may also check the pulse in your feet to assess blood flow.
Laboratory Tests
The healthcare provider may order laboratory tests to check for infection or other underlying conditions contributing to the foot ulcer's development. These tests may include a complete blood count (CBC) or a wound culture to identify the type of bacteria present in the wound.
Imaging Tests
Imaging tests such as X-rays, ultrasound, or MRI may be ordered to assess the extent of the foot ulcer and to check for underlying issues such as bone infection or vascular problems.

Treating Foot Ulcers
Treatment for foot ulcers will depend on the severity of the wound and any underlying conditions contributing to the development of the ulcer. Options may include:
Medical Management
Medical management of foot ulcers may include the following:
- Wound care: Proper wound care is essential for healing foot ulcers. This may include cleaning the wound with gentle soap and water, applying a dressing to protect the wound, and keeping the wound moist to promote healing. Your healthcare provider may recommend a specific type of dressing for your wound, such as a hydrogel or alginate dressing.
- Debridement: Debridement is the process of removing dead or damaged tissue from the wound. This can be done surgically or with medications such as enzymes or maggots. Debridement can help stimulate healing and prevent the ulcer from becoming infected.
- Antibiotics: If the foot ulcer is infected, your healthcare provider may prescribe antibiotics to help clear the infection. It is important to take the antibiotics as directed to ensure the infection is fully treated.
- Pain management: Foot ulcers can be painful, and your healthcare provider may recommend medications to help manage the pain.
Surgical Options
Surgical intervention may sometimes be necessary to treat a foot ulcer. Options may include:
- Skin grafting: Skin grafting involves taking a piece of healthy skin from another part of the body and attaching it to the foot ulcer. This can help the ulcer heal more quickly.
- Amputation: In severe cases, amputation may be necessary to prevent the spread of infection or to prevent further damage to the foot.

Home Care and Prevention
There are several steps you can take at home to help prevent foot ulcers and to manage them once they occur:
- Keep your feet clean and dry: Wash your feet daily with gentle soap and water, and dry them thoroughly, especially between the toes.
- Wear properly fitting shoes: Shoes that fit well and offer support can help prevent foot ulcers from developing. Avoid going barefoot or wearing shoes that are too tight or too loose.
- Inspect your feet daily: Check your feet daily for any cuts, blisters, or other wounds, and seek medical attention if you notice any changes.
- Manage your diabetes: Proper management of diabetes is essential for preventing foot ulcers. This includes checking your blood sugar levels, getting regular check-ups, and following a healthy diet and exercise plan.
When to See a Doctor
If you have diabetes or are at risk for foot ulcers, you must see a healthcare provider regularly to check for any signs of a developing ulcer. If you notice any changes in your feet, such as a wound that is not healing or redness or swelling, you should also seek medical attention as soon as possible.
Conclusion
Foot ulcers can be painful and difficult to heal, but they can be managed effectively with proper treatment and care. If you have diabetes or are at risk for foot ulcers, it is important to prevent these wounds from developing, such as wearing properly fitting shoes, checking your feet daily, and managing your diabetes. If you develop a foot ulcer, it is important to seek medical attention and follow your healthcare provider's treatment plan to ensure that the ulcer heals properly and prevents further complications.
FAQ
What is the best thing to put on a foot ulcer?
The best thing to put on a foot ulcer will depend on the specific needs of the wound. In general, a moist wound healing environment is preferred as it can help promote healing and prevent scar tissue formation. Your healthcare provider may recommend a specific type of dressing, such as a hydrogel or alginate dressing, to help keep the wound moist.
Should a foot ulcer be kept moist or dry?
A foot ulcer should generally be kept moist to promote healing. Dry wound healing environments can slow the healing process and increase the risk of scarring.
How long should it take a foot ulcer to heal?
The length of time it takes for a foot ulcer to heal will depend on the size and depth of the wound and any underlying conditions that may be affecting healing. In general, foot ulcers can take several weeks to several months to heal, depending on the case's specifics.
How often should you change the dressing on a foot ulcer?
The frequency of dressing changes will depend on the specific needs of the wound and the type of dressing being used. In general, dressings should be changed every 1-3 days or more frequently if they become soiled or wet. Your healthcare provider can advise you on the appropriate frequency of dressing changes for your specific case.
How do you dress a foot ulcer wound?
To dress a foot ulcer wound, follow these steps:
- Wash your hands thoroughly with soap and water.
- Clean the wound with gentle soap and water or as directed by your healthcare provider.
- Apply a thin layer of wound healing ointment if your healthcare provider recommends it.
- Place the dressing over the wound, ensuring it covers the entire wound.
- Secure the dressing in place with adhesive tape or bandages.
- Change the dressing according to the frequency recommended by your healthcare provider.
It is important to follow your healthcare provider's instructions for dressing the wound and to seek medical attention if the wound does not appear healing or if you notice any signs of infection.

