The Role of Skin Grafts in Healing Diabetic Foot Ulcers
Diabetic foot ulcers are a common and serious complication of diabetes, and effective treatment is essential to prevent serious complications such as amputation. One option for the treatment of diabetic foot ulcers is the use of skin grafts, which can provide a protective barrier, facilitate the growth of healthy skin, and improve the appearance of the wound. This article will explore the role of skin grafts in treating diabetic foot ulcers, including the different types of skin grafts, the benefits and risks of the procedure, and the factors that may affect the success of a skin graft. We will also discuss the high costs of skin substitutes and grafts and the importance of seeking medical attention for diabetic foot ulcers.
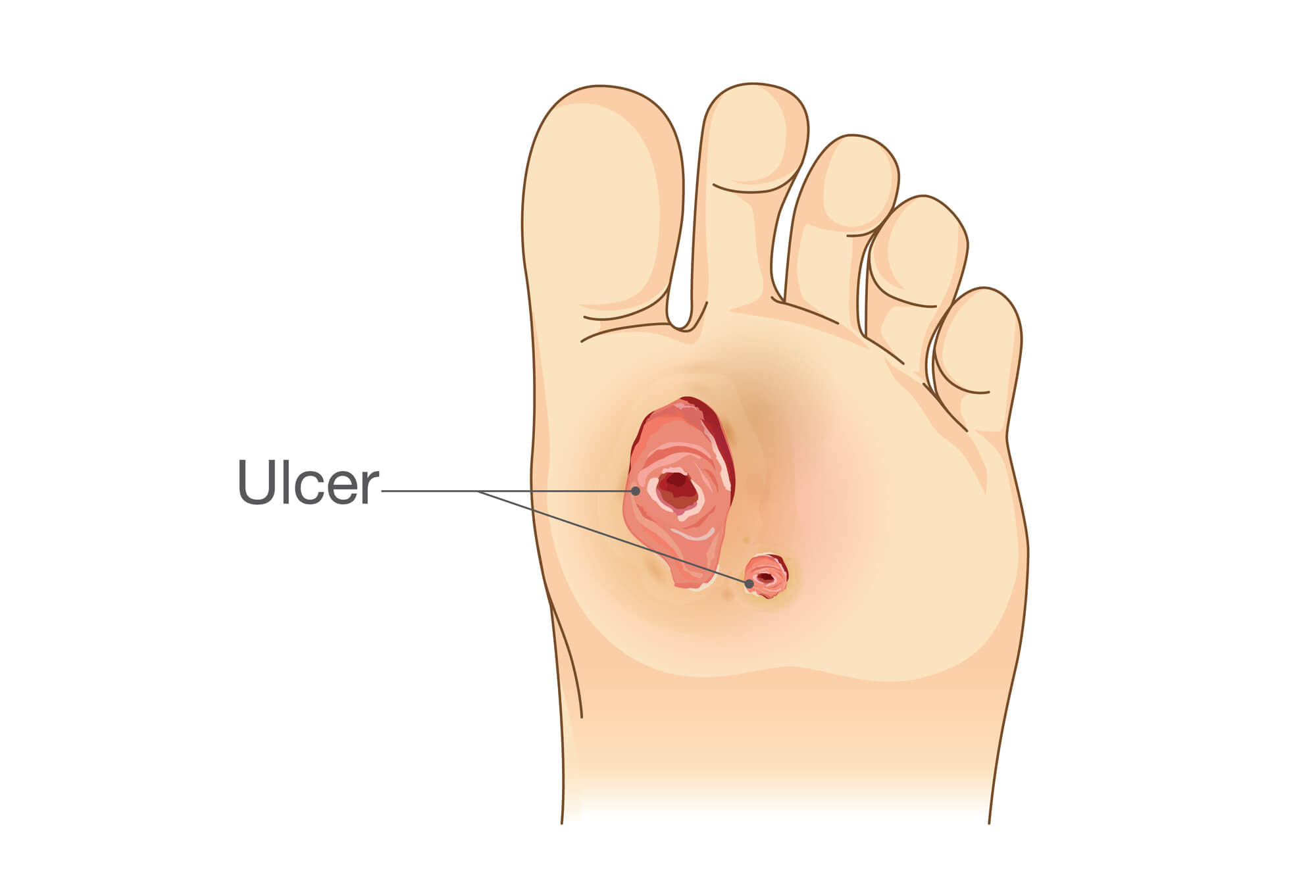
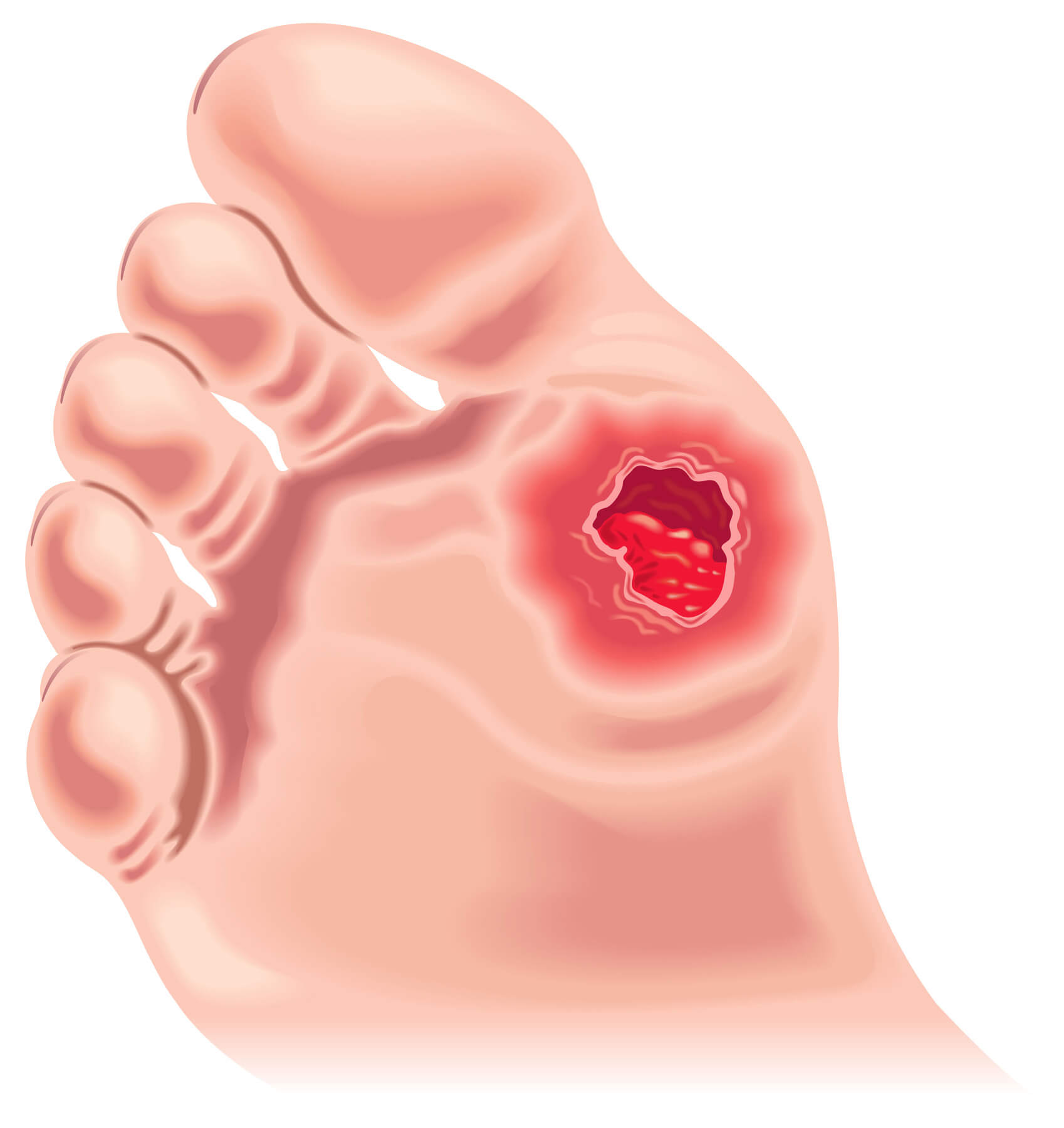
What Are Diabetic Foot Ulcers?
Diabetic foot ulcers are sores or wounds that develop on the feet of people with diabetes. They can be caused by various factors, including poor circulation, nerve damage, and excess pressure on certain areas of the foot. These ulcers can be slow to heal and can lead to serious complications if left untreated, such as amputation or even death.
The Importance of Timely Treatment
Diabetic foot ulcers require prompt and effective treatment to prevent the risk of complications. This may involve wound care, medication, and in some cases, surgery. The earlier a foot ulcer is detected and treated, the greater the chance of successful healing and a positive outcome.
What Are Skin Grafts?
A skin graft is a surgical procedure in which a piece of skin is removed from one area of the body (called the donor site) and transplanted into another area (called the recipient site). Skin grafts can cover wounds or injuries that are not healing properly or repair skin damage caused by burns or other injuries.
How Skin Grafts Are Harvested
There are several methods for harvesting skin for grafting, including split-thickness grafting, full-thickness grafting, and composite grafting. In split-thickness grafting, only the top layers of the skin are removed, while in full-thickness grafting, the entire thickness of the skin is removed. Composite grafts involve the removal of skin, fat, and blood vessels from the donor site.
Types of Skin Grafts
There are several types of skin grafts, including autografts, allografts, and xenografts. Autografts are skin grafts taken from the patient's body, while allografts are taken from a donor of the same species. Xenografts are taken from a different species, such as a pig. Autografts are considered the gold standard for skin grafting, as they have a lower risk of rejection and a higher success rate than other skin grafts.
How Skin Grafts Can Help Heal Diabetic Foot Ulcers
Providing a Protective Barrier
One of the main benefits of skin grafts for diabetic foot ulcers is that they provide a protective barrier over the wound. This can help prevent infection and protect the wound from further damage. Skin grafts can also help reduce the risk of scarring and improve the appearance of the wound.
Facilitating the Growth of Healthy Skin
Another benefit of skin grafts is that they can help facilitate the growth of healthy skin at the wound site. This can help speed up the healing process and improve the chances of a successful outcome.
Potential Complications of Skin Graft Procedures
As with any surgical procedure, skin grafts carry a risk of complications. These may include infection, bleeding, scarring, and reactions to the anaesthesia. There is also a risk of the graft failing to take, which may require additional surgery to correct.
Factors that May Affect the Success of A Skin Graft
Several factors can affect the success of a skin graft, including the patient's overall health, the size and location of the wound, and the quality of the donor site. It is important to discuss these factors with a healthcare professional, such as a podiatrist or a wound care specialist, to determine the best course of treatment.
Conclusion
skin grafts can be an effective treatment option for diabetic foot ulcers, providing a protective barrier and facilitating the growth of healthy skin. While skin grafts are generally considered safe and effective, patients need to be aware of the potential risks and complications involved and the high costs of these products. It is also crucial for people with diabetes to seek timely medical attention for diabetic foot ulcers and follow the recommended treatment plan to achieve the best possible outcome and prevent serious complications.
FAQ
How long does a skin graft take to heal on the foot?
The healing time for a skin graft on the foot can vary depending on several factors, including the size and location of the wound, the patient's overall health, and the quality of the donor site. In general, skin grafts on the foot take longer to heal compared to other parts of the body due to the weight-bearing nature of the foot and the potential for increased pressure on the graft. Wound healing can also be slowed by factors such as poor circulation and underlying medical conditions like diabetes. On average, it can take several weeks to months for a skin graft on foot to fully heal.
When can I walk after foot skin graft?
The ability to walk after a foot skin graft depends on the location and size of the graft, as well as the patient's overall health. In some cases, patients may be able to walk immediately after the grafting procedure, while in others, a period of the non-weight bearing may be required. It is important to follow your healthcare team's recommendations and not put weight on the graft until it has fully healed.
Can you do a skin graft on the bottom of your foot?
Yes, it is possible to do a skin graft on the bottom of the foot, also known as the plantar surface. This may be necessary to cover a wound or injury on the bottom of the foot or repair skin damage caused by burns or other injuries. Skin grafts on the bottom of the foot may take longer to heal compared to other parts of the body due to the weight-bearing nature of the foot and the potential for increased pressure on the graft. It is important to follow your healthcare team's recommendations and not put weight on the graft until it has fully healed.

