Why Do I Have Heel Pain?
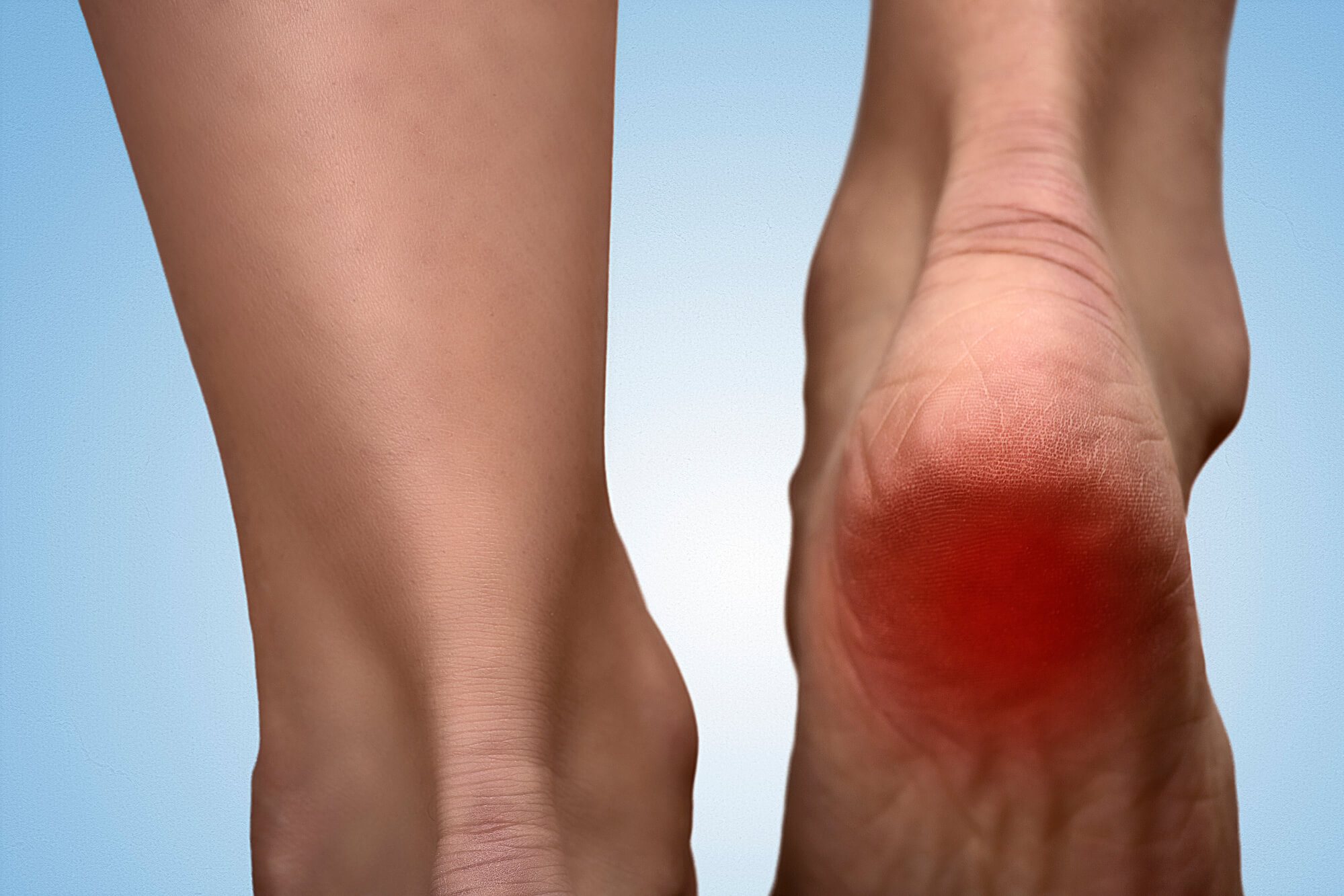
Heel pain is a common problem that affects people of all ages. Various factors, including injuries, overuse, and medical conditions, can cause it. If you experience heel pain, seeking medical attention to identify the cause and get proper treatment is essential. This article will discuss the most common causes of heel pain, including plantar fasciitis, Achilles tendonitis, bursitis, and heel spurs. We will also explore the diagnosis and treatment options available to manage this condition.
Plantar Fasciitis: The Most Common Cause of Heel Pain
Plantar fasciitis is the most common cause of heel pain, accounting for approximately 80% of cases. It is a condition that occurs when the plantar fascia, a thick band of tissue that connects the heel bone to the toes, becomes inflamed. Plantar fasciitis often develops gradually over time and can be caused by overuse, especially in athletes, or from standing or walking for long periods on hard surfaces. Symptoms of plantar fasciitis include sharp pain in the bottom of the foot or the heel, especially when standing or walking. The pain may also worsen in the morning or after sitting for long periods.
Treatment options for plantar fasciitis include rest, ice, compression, and elevation (RICE) to reduce inflammation and pain. Physical therapy may also be recommended to stretch and strengthen the calf muscles and plantar fascia. Shoe inserts or orthotics can also provide support and cushioning to the foot, reducing pressure on the plantar fascia. In some cases, anti-inflammatory medications or steroid injections may be prescribed to manage the pain and inflammation. If conservative treatments fail to provide relief, surgery may be required to release the plantar fascia.

Other Causes of Heel Pain
In addition to plantar fasciitis, there are several other causes of heel pain, including:
- Achilles Tendinitis: This condition occurs when the Achilles tendon, which connects the calf muscles to the heel bone, becomes inflamed. It is often caused by overuse or a sudden increase in activity level. Symptoms of Achilles tendinitis include pain and stiffness in the back of the heel, especially in the morning or after physical activity.
- Heel Spurs: Heel spurs are bony growths that can develop on the underside of the heel bone. They are often caused by long-term strain on the plantar fascia or Achilles tendon. Heel spurs can cause pain when walking or standing.
- Bursitis: Bursitis is a condition that occurs when the bursa, a fluid-filled sac that cushions the joints, becomes inflamed. Repetitive motions, overuse, or injury can cause it. Bursitis symptoms include pain, swelling, and tenderness in the affected area.
- Tarsal Tunnel Syndrome: Tarsal tunnel syndrome occurs when the tibial nerve, which runs through a narrow passageway in the ankle, becomes compressed or pinched. It can cause pain, numbness, and tingling in the heel and foot.
- Fat Pad Atrophy: Fat pad atrophy is a condition that occurs when the fat pad on the bottom of the foot thins out, causing pain and discomfort when walking or standing.
- Neuropathy: Neuropathy is a condition that affects the nerves and can cause pain, numbness, and tingling in the feet and heels. It is often caused by diabetes or other medical conditions.

Diagnosing Heel Pain
A podiatrist typically begins with a physical examination of the foot and ankle when diagnosing heel pain. During this examination, the podiatrist will look for inflammation, swelling, or other abnormalities in the affected area. They will also assess the patient's gait, or how they walk, to identify any problems with foot or ankle mechanics contributing to the heel pain.
In addition to the physical examination, the podiatrist will also consider the patient's medical history, lifestyle factors, and symptoms when diagnosing. For example, they may ask the patient about their occupation, exercise habits, and footwear choices to identify potential risk factors for developing heel pain. They may also ask about the onset and duration of the pain and other symptoms, such as numbness, tingling, or weakness in the foot or ankle.
If the cause of the heel pain is not immediately apparent, the podiatrist may recommend additional imaging tests to assess the bones and soft tissues of the foot and ankle. X-rays can assess the structure of the foot and ankle and look for signs of bony abnormalities such as heel spurs. MRI or ultrasound may be used to assess the soft tissues of the foot and ankle, including the muscles, tendons, and ligaments. In some cases, nerve conduction studies may be recommended to assess nerve function in the foot and ankle and identify any underlying nerve-related problems contributing to the heel pain.
Overall, a thorough physical examination and assessment of medical history and symptoms are crucial for accurately diagnosing the underlying cause of heel pain. By taking a comprehensive approach to diagnosis, a podiatrist can develop an effective treatment plan to manage the pain and improve the patient's overall foot and ankle health.
Treatment Options for Heel Pain
The treatment options for heel pain depend on the underlying cause. In addition to the conservative treatments mentioned above for plantar fasciitis, Achilles tendinitis, bursitis, and other causes of heel pain may also respond to physical therapy to stretch and strengthen the affected muscles and tendons. Other non-surgical treatment options may include:
- Medications: Anti-inflammatory medications such as ibuprofen or naproxen may be recommended to reduce pain and inflammation.
- Steroid injections: Steroid injections can reduce inflammation and pain in the affected area.
- Extracorporeal Shock Wave Therapy (ESWT): ESWT is a non-invasive treatment that uses sound waves to break up scar tissue and promote healing.
- Surgery: If conservative treatments fail to provide relief, surgery may be necessary to repair damaged tissues or release tight ligaments.
Prevention of Heel Pain
Prevention of heel pain involves taking steps to reduce the risk of injury and overuse. The following preventive measures may help:
- Wear supportive shoes that fit well and provide adequate cushioning and arch support.
- Use shoe inserts or orthotics to provide additional support and cushioning.
- Stretch regularly, especially before and after exercise, to keep the calf muscles and plantar fascia flexible.
- Gradually increase activity levels to avoid overuse injuries.
- Maintain a healthy weight to reduce stress on the feet and ankles.
- Avoid standing or walking on hard surfaces for long periods.
- Get regular checkups with a podiatrist to identify and address any potential foot and ankle problems early.
Conclusion
Heel pain is a common problem caused by various factors, including injuries, overuse, and medical conditions. Plantar fasciitis is the most common cause of heel pain, but several other conditions can cause pain in the heel and foot. If you experience heel pain, it is important to seek medical attention to identify the cause and get proper treatment. Treatment options may include conservative measures such as rest, ice, and physical therapy or more invasive measures such as surgery. Progressively preventing heel pain involves reducing the risk of injury and overuse, including wearing supportive footwear, stretching regularly, and maintaining a healthy weight. With proper care and attention, most cases of heel pain can be successfully managed.

